A List of the Top 13 Game-Changing Apps making Patient Care Easier
In an era where technological advancements are reshaping almost all industries, medical providers at all stages of their career find themselves at the forefront of a digital revolution. With the ever-increasing demands on their time and aptitude, even the most tireless and dedicated doctors need tools that enhance their medical practice. That is why quick, accurate, and up to date medical information is so important in our day-to-day lives. We need apps that can streamline workflows and ultimately provide better care for patients.
To help in this pursuit, I have compiled a list of the best apps that can make our lives a little easier. These apps have helped many navigate the complex landscape of modern medicine.
These apps were chosen based on the level of accuracy, ease of use, the breadth of resources, and my colleagues’ experiences with using these apps. Although this list is carefully assembled and intended to help the reader, it cannot incorporate the expansive variety of medical apps available today.
Let’s delve into the realm of indispensable tools that shape healthcare delivery and continuing medical education!
1. AHRQ EPSS
AHRQ’s Electronic Preventive Services Selector, or AHRQ EPSS, empowers physicians with Evidence-Based Clinical Guidelines.
In the fast-paced world of medicine, having access to reliable and up-to-date clinical guidelines is essential for physicians to deliver optimal patient care. The AHRQ (Agency for Healthcare Research and Quality) Electronic Preventive Services Selector (EPSS) application is a powerful tool that provides us with evidence-based clinical guidelines!
Features and Functionality
This application is designed to assist healthcare providers in identifying appropriate preventive services for their patients based on age, sex, and risk factors. The application covers a wide range of preventive services, including appropriate screenings based on age and gender, and immunizations. It incorporates recommendations from peer reviewed and vetted sources such as the U.S. Preventive Services Task Force (USPSTF), the Centers for Disease Control and Prevention (CDC), and the Advisory Committee on Immunization Practices (ACIP).
The user-friendly layout of the EPSS application allows for simple navigation and quick access to pertinent instructions.
This application has a nice feature where you can input patient-specific data like age, sex, and risk factors and it will generate a list of suggested preventive services based on the most recent research and recommendations. The recommendations are broken down by age group and give a thorough justification for or against each preventive therapy, as well as the frequency, screening methods, and potential advantages and disadvantages.
Reliable and Accurate Searches
Users can use the search feature in the AHRQ EPSS application to find specific guidelines quickly or to browse through categories based on demographics. Additionally, the tool has bookmarking and history features that let doctors easily access previously read advice and preserve commonly used ideas. What’s more, the guidelines presented in the EPSS application are very organized and easy to understand.
Each recommendation includes a summary of the evidence, grading of the recommendation, and links to relevant supporting documents and resources.
The AHRQ EPSS application is widely recognized for its reliability and accuracy. Hence, the recommendations provided are evidence-based and incorporate the best available evidence at the time of publication. It also includes references to the source guidelines, allowing healthcare professionals to verify the information and delve deeper into the supporting evidence if desired.
With its user-friendly interface, comprehensive recommendations, and up-to-date information, the application empowers physicians to make informed decisions regarding preventive care. This is an essential tool for physicians because it enhances the delivery of preventive services and ultimately improves patient outcomes.
Whether you are a primary care physician, specialist, or medical student, incorporating the AHRQ EPSS application into your clinical practice will undoubtedly support you in providing evidence-based preventive care to your patients.

2. Doximity
Doximity is a widely recognized and trusted social networking platform for healthcare professionals. Since its inception in 2010, this application has become a game-changer. This application fulfills various needs such as providing seamless communication, knowledge sharing, and professional networking within the medical community.
Features and Functionality
Doximity offers a wide range of features specifically tailored to the needs of health care providers among which are a) the provision of a secure and HIPAA-compliant platform for physicians to connect, collaborate, and communicate with their peers, b) a comprehensive physician directory, allowing users to search and connect with colleagues, specialists, and potential collaborators, and c) Doximity incorporates features such as secure messaging, voice calling, and video conferencing, enabling efficient and confidential communication among healthcare professionals.
Doximity’s Newsfeed, which curates and offers medical news, research updates, and expert insights specific to the user’s specialization and interests, is a standout feature because it encourages continued medical education, and keeps healthcare professionals up to date on the most recent developments in their professions.
Doximity also provides a forum for doctors to exchange case studies, medical views, and research findings, encouraging intellectual engagement and collaboration.
Easy to Use
Furthermore, Doximity boasts a user-friendly interface, making it accessible and intuitive for clinicians at any stage of tech expertise to navigate and utilize its features.
Some more of its features include:
a) The app allows users to customize their profiles, highlight their expertise, and display professional achievements.
b) The search functionality enables easy discovery and connection with colleagues, specialists, and potential mentors or mentees.
c) The messaging and calling features are seamlessly integrated, allowing for real-time communication and collaboration without compromising patient privacy or data security.
d) The platform also provides options to save articles, bookmark research papers and follow key opinion leaders further tailoring the user experience and facilitating ongoing learning.
Collaborate and Communicate
Doximity has significantly impacted the way healthcare professionals collaborate and communicate. The application has bridged geographical barriers, enabling physicians to consult, and share expertise with colleagues across the globe.
Furthermore, Doximity has proven to be invaluable in physician recruitment and job opportunities.
The platform facilitates professionals who are seeking employment to explore career opportunities, connect with potential employers and stay updated on job openings. This not only benefits individual physicians but also contributes to the overall growth and advancement of the medical community.
Doximity is very useful because it facilitates communication and networking. It offers a secure platform for healthcare professionals to connect, share knowledge, and advance their careers.
One of the best features about this application is that it allows for a free phone and fax number that can be shared with patients and colleagues. As the healthcare landscape continues to evolve, Doximity’s impact on enhancing collaboration and improving access to healthcare patient care will ultimately contribute to excellent healthcare delivery.
3. DynaMed
This is an indispensable medical application that serves as a comprehensive resource for healthcare providers. With its extensive collection of evidence-based content, it covers a wide range of medical specialties and topics, making it an essential tool for clinicians, students, researchers, and educators.
Features and Functionality
One of the key benefits of DynaMed is its commitment to regular updates allowing practitioners to stay current with the latest research findings, clinical guidelines, and treatment recommendations. Its created to ensure speed and efficiency of navigation allowing users to find the information they need with ease. Its intuitive layout and organization make it effortless to locate relevant clinical data regardless of the practitioners age and comfort with medical technology.
This application makes diagnosing complex cases and formulating treatment plans much easier. Furthermore, DynaMed offers various interactive tools and calculators that assist in clinical decision-making, from risk assessment tools to medical calculators and serves as a trusty peripheral brain!!
The benefits of using DynaMed extend beyond individual patient care. The app promotes evidence-based medicine, encouraging healthcare providers to base their decisions on sound scientific research. By accessing trustworthy and up-to-date information, clinicians can improve the overall quality of healthcare delivery.
DynaMed is a must-have resource for anyone seeking reliable and current clinical information.

4. DynaMedex
This comprehensive and esteemed application serves as an invaluable resource in the field of clinical decision support. DynaMedex is a beacon of evidence-based medicine offering a vast collection of peer-reviewed literature.
It is a great resource for accessing clinical guidelines. Its meticulous and rigorous approach to information gathering ensures that healthcare providers have access to the most current and trustworthy medical information available.
Features and Functionality
One of the app’s standout features is its commitment to regularly updating its content, ensuring that healthcare professionals can rely on the most recent advancements and insights.
Moreover, DynaMedex excels in its user-friendly interface enabling seamless navigation through its wealth of medical information. Its design allows healthcare professionals to quickly retrieve relevant clinical information and save precious time. This application is designed to facilitate informed decision-making at the point of care.
Furthermore, the app’s filtering options empower users to refine their queries and pinpoint the most pertinent information for their specific clinical scenarios. This capability contributes significantly to enhancing diagnostic accuracy.
Its commitment to evidence-based medicine, regular updates, and powerful search capabilities makes it an indispensable tool for healthcare providers across all specialties.
5. Epocates
If you’re looking for a free and efficient tool to aid in choosing a specific drug, look for med-med interactions, or look up safety of a particular drug in pregnancy, look no further. One such tool that will deliver this and more is the Epocrates application.
Features and Usability
The Epocrates application offers a wide range of features designed to assist us in daily practice. Available on both iOS and Android platforms, the app facilitates easy navigation and quick access to essential drug information.
It features CME learning and allows access to more than 600 calculators.
It provides comprehensive drug information including dosing guidelines, indications, contraindications, adverse effects, drug interactions, and even pill identification. The content is regularly updated, ensuring that physicians have access to the most current information.
The app also provides disease monographs, guidelines, and diagnostic tools and other tools such as risk score calculators.
There is a paid version that is extremely comprehensive and it allows access to OTC products and alternative medicine therapies. Epocrates also allows quick access to multiple drug coverage plans, which translates into less drug benefit denials.
Best of all, the intuitive design ensures that physicians of all experience levels can utilize the app with ease.
Is the free version better??
While the Epocrates app provides a wealth of valuable information, it is essential to note its limitations.
The free version offers more limited access to advanced features requiring a paid subscription. While the subscription cost may be a barrier for some healthcare professionals, the app’s value and convenience justify the expense.
6. Evernote
Although it is not geared specifically toward healthcare providers, Evernote is the ultimate digital workspace for capturing, organizing, and sharing your ideas and information.
Features and Usability
This application is useful because it helps you stay on top of your game and achieve your goals.
Evernote lets you keep your notes, web pages, files, and images in one place, and access them from anywhere. Whether you’re a medical student, resident, or a practicing clinician, Evernote can help you capture any document or picture such as an EKG or an x-ray and scan the document, add attachments, and sync pictures, articles and even your drawings to other devices.
This is an app that helps you remember everything and stay organized. Best of all your documents are stored in one place and can be accessed on the go!
In short, Evernote helps streamline information and does away with redundancy, which in the end saves valuable time and energy.
7. MD Calc
MD Calc is a comprehensive and reliable medical reference application that offers a vast array of calculators, risk scores, and decision support tools. One of the developers of this application is Dr. Ian Stiell who also developed the Ottawa Ankle Rule.
Features and Functionality
MD Calc is a mobile application designed to assist clinicians make evidence-based medical decisions. It holds a 4.9 out of 5 rating in the IOS app store.
The application is known for the vast array of medical calculators that are kept up to date. In addition to medical calculators, you can access easy to use risk scores calculators and algorithms available on many topics. It helps with diagnosis and treatment. It has guides that help rule out medical conditions.
This app allows physicians to input patient-specific data and obtain risk assessments, diagnostic probabilities, medication dosages, and more.
With this application, you can access a diverse range of calculations, including but not limited to, CHA2DS2-VASc score, APACHE II score, GFR estimation, and opioid conversion calculations. Furthermore, MD Calc incorporates predictive models and algorithms that aid in clinical decision-making, which in turns improves patient outcomes.
Features Galore!
Additionally, MD Calc offers the option to save frequently used calculators as favorites further streamlining the workflow for physicians.
Another wonderful feature of MD Calc is that it provides comprehensive interpretations of results, including explanations of the underlying formulas and references to relevant medical
MD Calc streamlines clinical decision-making and promotes evidence-based medicine. It has become a trusted companion for physicians, contributing to improved patient care and outcomes.
8. Medi Bubble
This application is a remarkable medical application designed to bridge the communication gap between healthcare providers and non-English speaking patients.
Features and Functionality
Its wide language database and user-friendly interface enable precise real-time translation of medical terminology and phrases. This tool is extremely useful in healthcare settings, as it improves patient-doctor relations and ensures proper information sharing. It currently holds a 4.3 out of 5 rating in the IOS app store.
It is HIPPA compliant and offers end-to-end encryptions of video communications.
Another perk this application offers is a fax capability that is also encrypted end-to- end.
A great benefit of this applications is that it allows accumulation of continuing medical education credits (CME).
Its user-friendly design and extensive language support make it a trustworthy resource for healthcare professionals, assisting with diagnosis, treatment planning, and patient education.
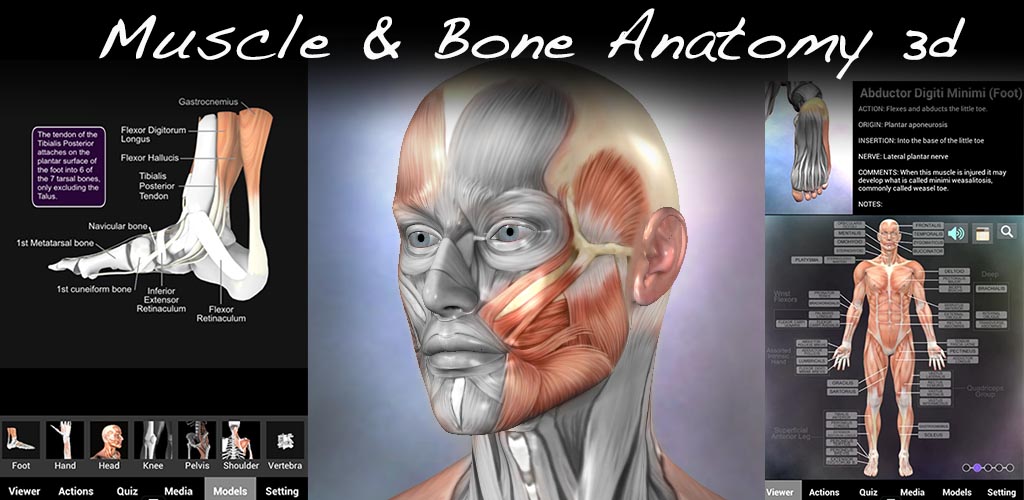
9. Muscle and Bone Anatomy in 3D
Muscle and bone anatomy in 3-D provides medical students, residents, and physicians with a powerful tool for accurate diagnosis, treatment planning, and patient education. It currently holds a 4.7out of 5 rating in the IOS app store.
Features and Functionality
By utilizing advanced imaging techniques and computer software, a three-dimensional representation of the musculoskeletal system can be generated. This allows for a detailed visualization of the relationship between muscles, bones, and surrounding structures. Imagine being able to visualize muscle movement in real time and in 3-D!! This app allows the user to learn from dissected anatomy, because it shows muscle, ligament, and tendon attachments.
Best of all, this application has quizzes you can take to test your level of knowledge and highlight areas that may need more attention. Hence, it is an excellent tool for learning.
Using this app makes identification of abnormalities, fractures, joint disorders, and muscle imbalances. much easier. Surgeons can plan surgical interventions with greater precision, optimizing outcomes and reducing surgical risks. Furthermore, this technology enables physicians to explain complex conditions to patients using interactive 3-D models, enhancing their understanding, and facilitating informed decision-making.
10. Pepid
Pepid is a highly regarded medical application that provides an extensive range of medical content, clinical tools, and decision support resources. It currently holds a 4.7 out of 5 rating in the IOS app store . This application made the list because it is very user friendly, offers a variety of tools, and is easy to access on the go. It is very useful for emergency room and urgent care physicians Here’s why:
Features and Functionality
Pepid boasts an impressive collection of clinical information, which allows you to look up differential diagnoses. It also offers clinical decision support tools, such as differential diagnosis generators, symptom checkers, and treatment algorithms. Pepid has a vast drug database including pill pictures and IV drug compatibility, and med-med-interaction information.
What I like about this application is its availability on multiple platforms. Other noteworthy feature is its varied medical content that is regularly updated.
Pepid assists with clinical decision making and treatment planning when time is of the essence.
Areas for Improvement??
If I could wave a magic wand and add features to this application, it would be the integration of multimedia resources such as images and videos that can be shared with colleagues and patients. Who knows, maybe this capability will soon be available on this application.
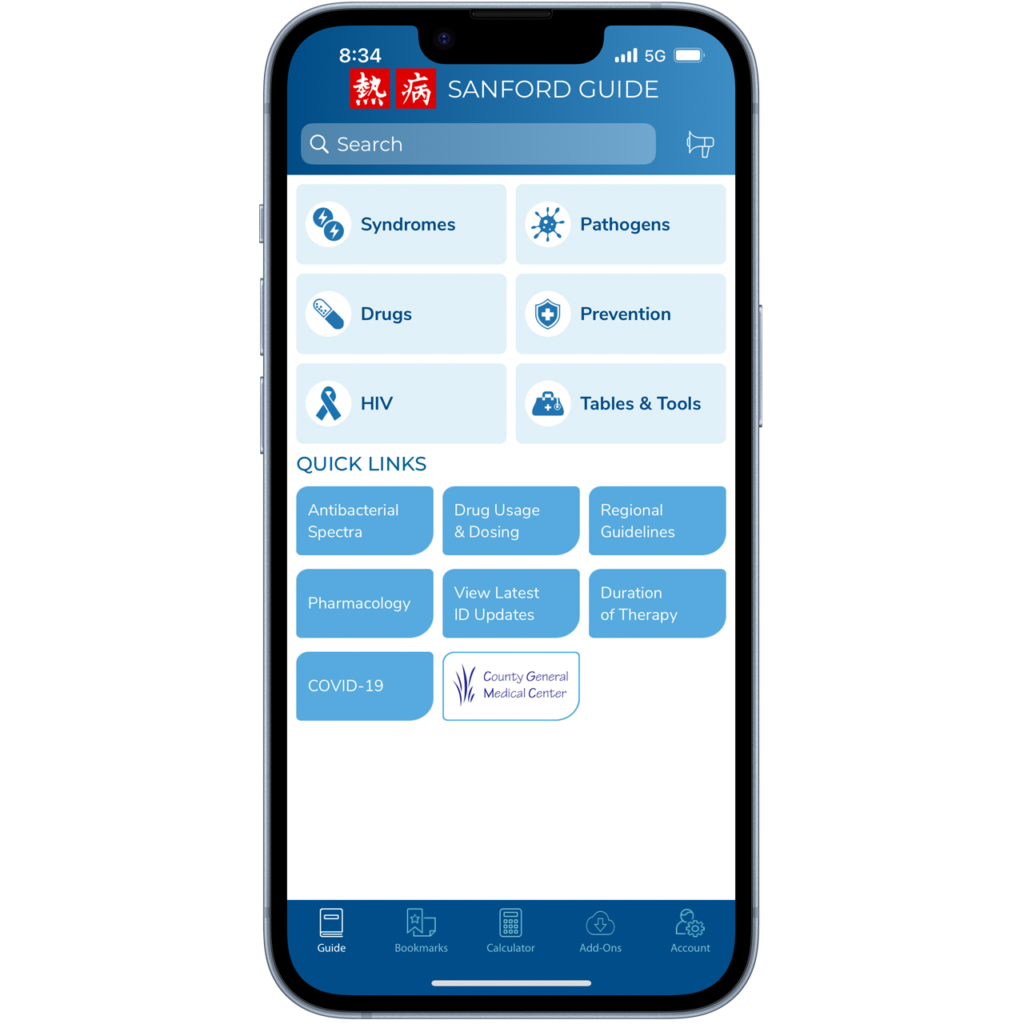
11. Sanford Guide to Antimicrobials Application
This user-friendly application has long been a favorite among clinicians across many specialties. Its comprehensive content and evidence-based recommendations make it a trusted resource for the treatment of infectious diseases. The Sanford Guide to Antimicrobials book has been in circulation since 1969. The app allows for much quicker access to the same information.
Features and Functionality
The Sanford Guide to Antimicrobials application boasts a user-friendly interface making it accessible to healthcare professionals at all levels of expertise. The app is available for both iOS and Android devices, ensuring compatibility across platforms. Its intuitive design allows for quick navigation, making it easy to find the information needed in a time-sensitive clinical setting.
The app’s most significant strength lies in its comprehensive coverage of antimicrobial therapies. It provides detailed information on various infectious diseases, including diagnosis, treatment options, dosing regimens, and management of complications. The content is regularly updated to reflect the most current guidelines and emerging infectious threats, ensuring accuracy and relevance.
The information is presented in a concise manner, allowing busy healthcare providers to access critical details without feeling overwhelmed.
For More Than Just Physicians
In addition to physicians, this app is very useful for pharmacists, and other healthcare personnel involved in antimicrobial therapy.
This app provides information on dose adjustment and treatment duration. The inclusion of information on drug interactions, adverse effects, and special populations enhances its relevance in the health care arena.
Moreover, the Sanford Guide to Antimicrobials application includes a range of supplementary features such as calculators for renal dosing, algorithms for infection management, and susceptibility data for specific pathogens.
Areas for Improvement??
While some users have complained about interface glitches, it holds a 4.8 out of 5 rating in the IOS app store. It’s important to note that updates to the interface have helped with these glitches. It is best to update the application as newer versions become available to avoid any technical issues.
Considering the app’s comprehensive content and regular updates, the price is justifiable for its value and the convenience it offers. I would recommend this application to medical students, residents, and fellows.
It is similarly very helpful for physicians, pharmacists, and Advanced Practice Clinicians.

12. UpToDate
This long beloved and trusted application enhances your expertise.
The application is easy to use and understand and in case of any technical issues, you can quickly turn to their top-notch customer support team and resolve any issues. It currently holds a 4 out of 5 rating in the IOS app store
Features and Functionality
This application is trusted by healthcare professionals worldwide due to its ability to deliver evidence-based guidance, comprehensive research, and expert opinions right at your fingertips. It is like always having your smartest residency preceptor with you.
UpToDate is very useful for accessing the most recent guidelines set forth by medical societies. It is very organized and features a table on contents that allows you to skip to the portion of the article you are interested in exploring, without wasting time reading through long articles.
With UpToDate, you can earn continuing medical education credits and address medical queries simultaneously.
This application is used by many practitioners to enhance patient care. Stay UpToDate as you quickly go about caring for patients.

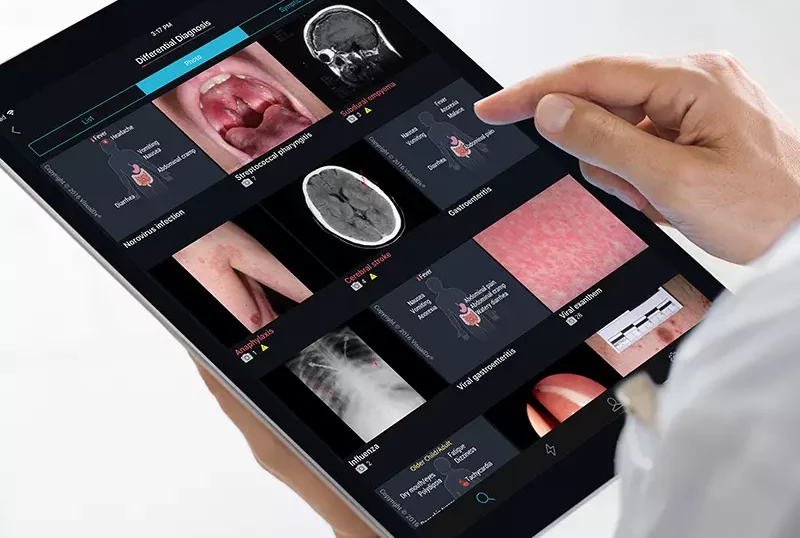
13. Visual Dx and Visual DX Plus Applications
Visual Dx and Visual DX Plus are two prominent apps that offer comprehensive image-based diagnostic support. Currently, it holds a 4.5 out of 5 ranking in the IOS app store. Both apps are available on iOS and Android platforms.
Features and Functionality
Visual Dx and Visual DX Plus provide an extensive collection of medical images, allowing clinicians to visually explore and compare various clinical presentations. These applications offer a user-friendly interface, making it easy to search for specific conditions, view images, and access relevant clinical information.
Of course, the strength of Visual Dx and Visual DX Plus lies in their extensive and diverse database of medical images. This allows the applications to provide high-quality visuals of various dermatological, ophthalmological, and general medical conditions. These images are accompanied by detailed clinical information, including differential diagnoses, diagnostic pearls, and treatment options. The content is regularly updated, incorporating the latest medical best practices.
Additional features of Visual DX Plus include access to a vast library of medical textbooks and journals, further augmenting its value and practicality.
Without a doubt, Visual Dx and Visual DX Plus continue to play a crucial role in facilitating accurate diagnoses, improving patient care, and supporting ongoing medical education. I highly recommend this application for those clinicians who are responsible for the training of students and residents!
The future of health care is here
The use of applications and AI is here to stay. When developed with the clinician in mind, these applications serve as a valuable resource for healthcare practitioners, across multiple specialties and health care settings. Though useful, applications cannot take the place of high-quality patient -provider interaction. Our carefully cultivated skills and knowledge remain the best tool in the delivery of compassionate health care.
Ela Grigorian, MD

Check out my book!! 100 Delicious Vegan Recipes to Prepare at Home: All the Inspiration You Need for a 4 Course Meal or Any Combination to Satisfy Your Cravings